What Is Depression?
Causes
Symptoms
Treatments
Prevention Techniques
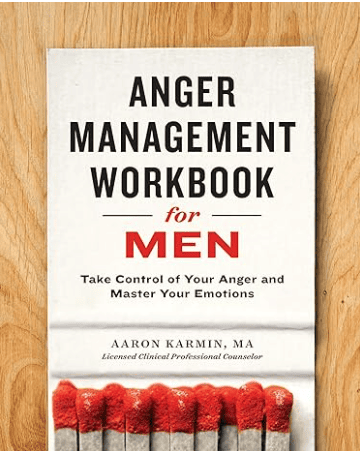
Helpful Products
What Is Depression?
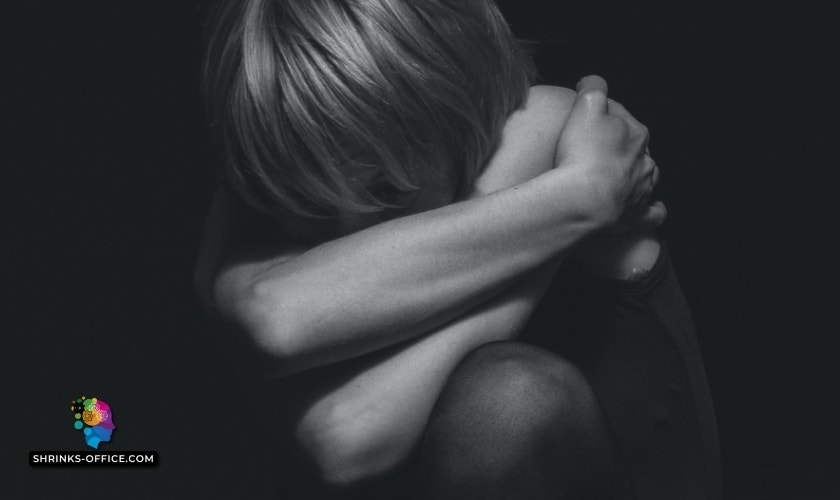
Depression is a mental health condition characterized by persistent sadness, hopelessness, and loss of interest in activities. It can also cause physical symptoms. Depression is a common condition that can range from mild to severe and can be treated with therapy, medication, or a combination of both.
Common Depression Causes
- Brain Chemistry
- Hormone Levels
- Family History
- Early Childhood Trauma
- Brain Structure
- Medical Conditions
- Substance Use
- Pain
- Insomnia Impact
- Guilt Or Worthlessness
Symptoms Of Major Depressive Disorder
- Persistent feelings of sadness, hopelessness, and/or worthlessness
- Loss of interest or pleasure in activities that were once enjoyed
- Significant changes in appetite and/or sleep patterns
- Difficulty concentrating, remembering, or making decisions
- Fatigue or loss of energy
- Feelings of guilt, worthlessness, or helplessness
- Thoughts of death or suicide
- Physical symptoms such as headaches or stomachaches that do not respond to treatment
- Irritability or agitation
Treatment Options For Depression
Medication
Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Psychotherapy
- Cognitive Behavioral Therapy
- Interpersonal Therapy
- Electroconvulsive Therapy (ECT)
- Light Therapy
- Mindfulness-based therapies
- Lifestyle changes
- Hypnosis
Prevention Techniques For MDD2
- Pets
- Eat Smart
- Foods That Boost Your Mood
- Exercise To Change How You Feel
- Exercise With Others For Support
- Get Enough Sunlight
- Make Time For Mindful Relaxation
- Get Involved In Your Community
- Keep Friends And Family In Your Life
- Get The Sleep You Need
- Avoid Alcohol And Drugs
- Stick To Your Treatment
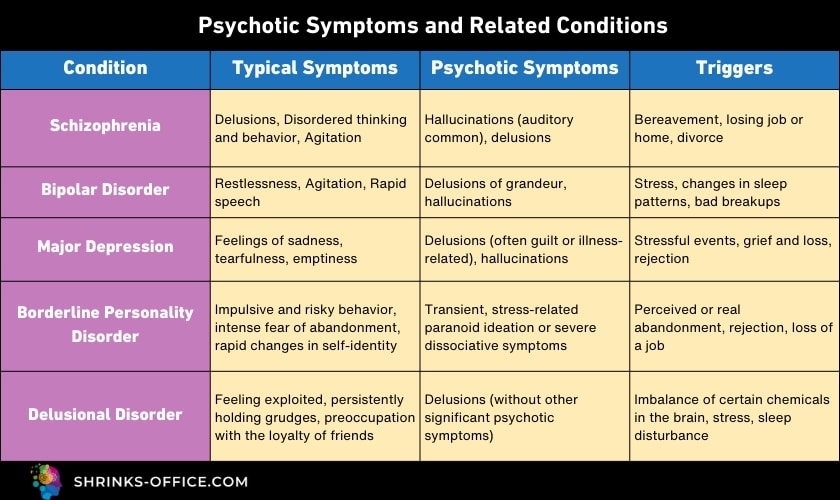
Depression comes in many forms, namely Major depressive disorder (MDD), Persistent depressive disorder, Bipolar depression, Premenstrual dysphoric disorder, Postpartum depression, Perinatal depression, and Psychotic depression, which range in severity and can affect anyone, regardless of age, race, or gender.
Over 200 million people are impacted by some or other depressive episode each year. It can cause intense sadness, apathy, and anxiety to become constant fixtures in your life. A persistent depressive disorder is characterized by intense feelings of sadness and despair that can last for weeks, months, or even years.
While there is no one cause of depressive disorders, it is believed to be the result of a combination of environmental and genetic factors.
Major depression can make everyday activities like going to work or school difficult and often leads to social isolation. If you think you may be suffering from severe depression, it’s important to seek help from a doctor or therapist. There are many treatments available that can help you manage your symptoms and improve your quality of life.
Depression causes
While the exact cause of a persistent depressive disorder is unknown, several factors may increase your risk of developing the condition.
Risk factors that can lead to depression include genetic or biological factors, stressful life events such as a death in the family or losing a job, medical conditions such as thyroid problems, drug and alcohol abuse, medications for other conditions, loneliness, and isolation from friends and family members, emotional and physical problems and anxiety disorders.
Depression is also more likely to occur if you have a close relative who has been diagnosed with depression by a mental health professional.
Common depression causes
People who have depression often experience major disruption in their brain chemistry which could lead them through episodes where they feel down or sad without knowing why.
Brain chemistry
An Appetite decrease along with behavior changes like impulsivity can last for days at a time. Parts of the brain that manage mood, sleep, appetite, thoughts, and behavior can have a chemical imbalance in people who have symptoms of depression.
Hormone levels
Changing hormones can lead to mild depression. Hormonal changes during your menstrual cycle or postpartum period may trigger symptoms. These include perimenopause and menopause and premenstrual disorders (PMS) when the levels of estrogen and progesterone change drastically in order for your body to prepare itself.
It also includes the period after childbirth has occurred, (confining period) the period your body needs to recuperate and recover from childbirth.
Immediately postpartum and the week following delivery, estrogen, and progesterone will both drop as our bodies need time away from those extra courses of hormones that affect moods negatively.
Simultaneously, there will be a surge in oxytocin (which is released in response to activation of sensory nerves during labor and breastfeeding) and prolactin, (the hormone that helps you make breastmilk).
These wildly swinging hormones are to blame for those two crazy postpartum depression, (also known as perinatal depression) facts you’ll experience after giving birth. However, this does come back around again once things normalize.
Studies show that when people are under physical stress like pain or restraint, oxytocin levels rise in the blood.
Although it’s always better to speak to a health care professional, we recommend this natural hormone supplement.
Family history
When a close family member, like a cousin or sister, has been diagnosed with depression, the odds of getting clinically depressed increase significantly, since genetics play an important role.
Early childhood trauma
Early childhood trauma can have lasting effects on your body’s ability to respond emotionally. Some events that happen in early life produce chronic fear responses and stress coping mechanisms which may be normal for some people, but not for others. An example of this would include being afraid of loud noises or crowds because you were raised with parents who always yelled at each other.
Want to know more about early childhood trauma, we recommend this book.
Brain structure
Brain structure and its role in depression have been a topic of great debate. The frontal lobe of your brain controls behavior, moods, and energy levels.
If this area is weaker than normal, it can lead to depression, but scientists aren’t sure if an individual begins displaying symptoms before or after a deficiency in the system occurs.
Medical conditions
It's critical to know the risks associated with certain medical conditions and how this may affect you. Sleep disorders such as insomnia or chronic pain increase your risk by 20-50%. Parkinson’s disease also poses a high hazard, while cancerous growths pose an even higher threat.
Medical conditions that can place somebody at a higher risk for MDD such as chronic pain or illness, fibromyalgia, chronic fatigue, heart disease and stroke, Parkinson’s disease, insomnia, cancer, Hypothyroidism, HIV, hormone imbalance, and postpartum depression.
Substance use
Although recreational drugs like alcohol, caffeine, and tobacco can influence your risk, it’s important to note that there are many factors involved when it comes to mental health disorders.
A history of alcohol or drug misuse by itself does not guarantee an increased incidence of mental illness, but rather suggests a correlation between these behaviors and potential future episodes. A history of substance or alcohol misuse can impact your risk.
Pain
People who feel emotional pain, or any physical pain for long periods of time, are significantly more likely to develop symptoms of depression.
The discomfort can become so overwhelming that it interferes with daily life activities, including work performance and social interaction.
People who experience emotional and physical problems for long periods of time are significantly more likely to develop, mental disorders and anxiety symptoms.
Insomnia impact
You might feel depressed because sleep disturbances such as insomnia (not being able to fall asleep, hard to stay asleep, or causing you to wake up too early and not be able to get back to sleep), make it difficult for some individuals with severe symptoms of depression (elevated mood) to get the rest they need. Over time, lack of sleep together with other causes can lead to MDD and lots of other medical illnesses.
Guilt or worthlessness
The Diagnostic Statistical Manual of the American Psychiatric Association (DSM-IV-TR) recognizes excessive or inappropriate guilt as one of the core symptoms of current MDD.
Sufferers with major depressive disorder (MDD) are more prone to experiencing moral emotions related to self-blame, such as excessive or inappropriate guilt and shame.
Feelings of guilt or worthlessness may overpower any sense that an MDD sufferer has about him- or herself. When we feel guilty, it usually means there was some sort of wrongdoing committed which causes considerable emotional pain.
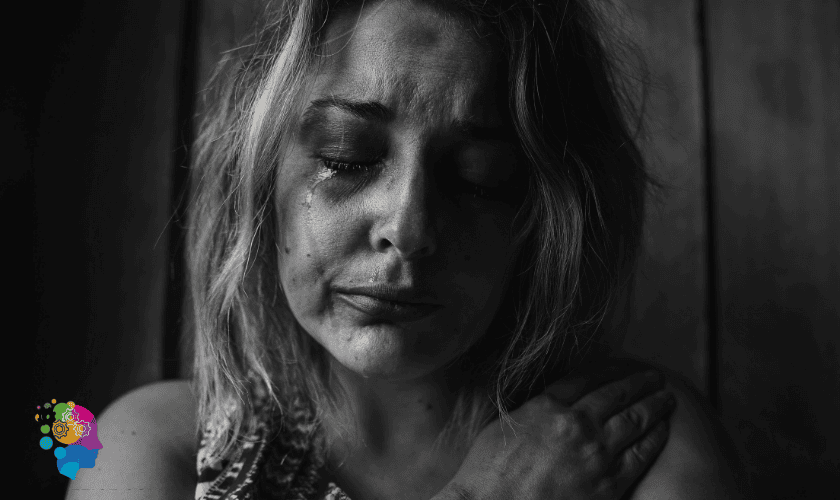
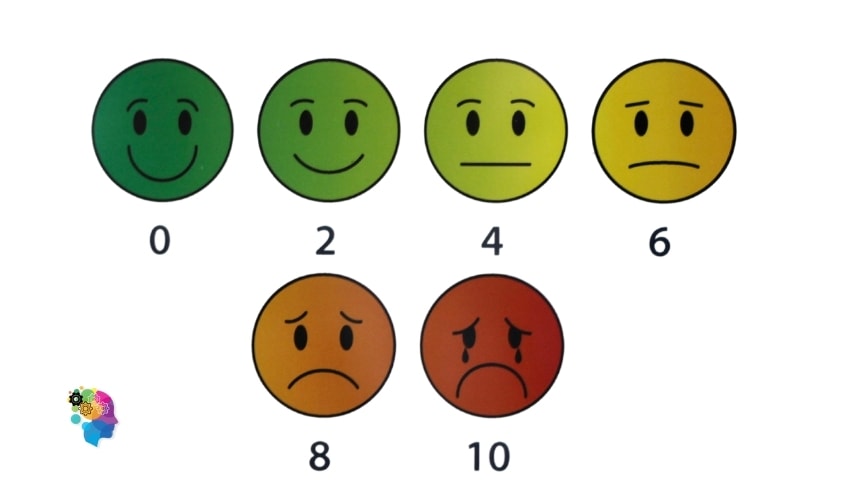
Symptoms of major depressive disorder
According to the DSM-IV-TR criteria for diagnosis; major depressive disorder is a very serious illness that can cause intense sadness, difficulty in thinking or concentrating, and decreased interest in activities that were once enjoyed.
When someone experiences persistent and intense feelings of sadness for extended periods, then they may have a mood disorder such as major depressive disorder (MDD).
Excessive or inappropriate guilt is one of the core symptoms of current MDD as per the Diagnostic Statistical Manual of the American Psychiatric Association (DSM-IV-TR). Sufferers with major depressive disorder (MDD) are more prone to experiencing moral emotions related to self-blame, such as excessive or inappropriate guilt and shame.
Other symptoms of major depressive disorder, according to the criteria found in DSM-IV-TR is as follows:
- A feeling of sadness and a depressed mood with decreased interest in activities that were once enjoyable.
- Inability to complete assignments at school/work due to lack of energy.
- Poor concentration.
- Weight gain
- Anxiety.
- Insomnia
- Irritability
- Suicidal thoughts
To be diagnosed with MDD, you need to meet the symptom criteria listed in DSM-5. This manual helps medical professionals diagnose mental health conditions and according to its criteria:
- You must experience a change in your previous functioning.
- Such change must occur for at least two or more weeks.
- Symptoms must either be a depressed mood or loss of interest in pleasurable activities previously enjoyed before the onset of the situation.
You should also experience 5 or more of the following symptoms in two weeks:
- You’re less interested in activities you previously enjoyed.
- You’re sad or irritable for most of your days, if not every day.
- You suddenly lose or gain weight, or your appetite changes significantly.
- You feel unusually tired and have a lack of energy.
- You frequently feel worthless or guilty about things that wouldn’t normally make you feel this way.
- You have a hard time concentrating, reasoning, or making decisions.
- You consider harming yourself or committing suicide.
- You can’t fall asleep or sleep more than usual.
- You feel restless.
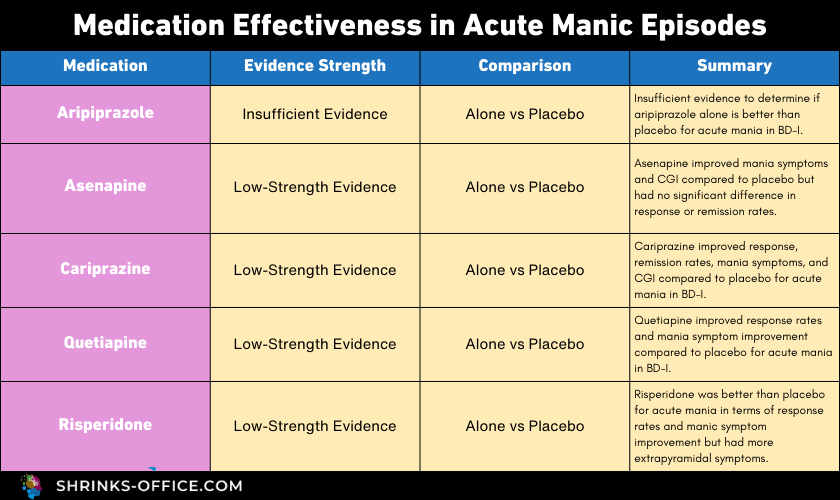
Treatment options for depression
Major Depressive Disorder and their effectiveness are based on research studies. Medication and psychotherapy are often used to deal with MDD. Some lifestyle changes may also assist in relieving certain symptoms.
People who suffer from severe MDD or are contemplating suicide may require hospitalization during therapy.
Outpatient treatment is also an option until symptoms improve.
Medications
Primary care providers usually begin (Major Depressive Disorder) MDD therapy by giving antidepressants.
Selective serotonin reuptake inhibitors (SSRIs)
Serotonin is a brain chemical that has been linked to mood. It may help to reduce anxiety and improve sleep habits.
Prozac, Celexa, Lexapro, and Zoloft are examples of SSRIs. SSRIs enhance the breakdown of serotonin in the brain, resulting in greater levels of this neurotransmitter.
Low serotonin levels are frequently associated with MDD and PDD (Persistent Depressive Disorder). By boosting the amount of serotonin in the brain, an SSRI can alleviate MDD and persistent depressive disorder symptoms.
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
(SNRIs) affects two important brain chemicals namely serotonin and norepinephrine. These drugs are sometimes called dual reuptake inhibitors or dual-acting antidepressants.
Norepinephrine is related to alertness and energy. Serotonin is associated with positive feelings of well-being and is also known as a feel-good chemical.
It’s believed that SNRIs help to treat depression by keeping up the levels of these two chemical messengers in your brain by stopping norepinephrine and serotonin from going back into the cells that released them.
SNRIs that are currently on the market:
- Desvenlafaxine
- Duloxetine
- Levomilnacipran
- Milnacipran
- Venlafaxine
SNRIs offers another option for tough-to-treat depression or depression with anxiety.
Other medications
Tricyclic antidepressants such as bupropion (Wellbutrin), may be used when other antidepressant medications haven’t helped.
Drugs like Provigil, which modulate the central nervous system and can reduce fatigue, are increasingly popular. They have a variety of adverse effects, including weight gain and drowsiness.
Benefits and drawbacks should be compared carefully with your doctor when taking any medication.
Types of therapy that may help depression
Psychotherapy
People with MDD can benefit from psychological therapy, also known as talk therapy. It entails seeing a mental health professional on a regular basis to discuss your illness and other related concerns.
Psychotherapy can help you:
- To pick an effective strategy for coping with any difficulties or other distressing occurrences like anxiety disorder, suicide attempts, and depressive symptoms.
- Discover new methods to cope with problems and solve issues.
- To learn how to boost your self-esteem.
- develop communication skills.
- To maintain a critical distance from your own experience and perceive yourself as an outsider. You should also approach situations in accordance with your principles instead of based on your feelings. By way of effective treatment to regain a sense of satisfaction and control in your life.
Cognitive behavioral therapy
Cognitive-behavioral therapy (CBT) is a type of psychotherapy. CBT is a blend of cognitive therapy and behavioral therapy. Cognitive therapy focuses on your moods and thoughts. Behavioral therapy specifically targets actions and behaviors.
Treatment usually entails finding more balanced and constructive ways to deal with stress with the help of mental health professionals. Therapy on a regular basis should help you cope with or get rid of distressing mental health issues or undesirable actions.
Counseling can also help manage Persistent depressive disorder (PDD, which is a type of Long term depression). Cognitive-behavioral therapy is often helpful for Persistent depressive disorder.
Interpersonal therapy
Therapists may employ a variety of approaches, such as role-playing, to assist clients to cope with their world. An interpersonal therapist will typically concentrate on the most pressing relational difficulties in order to help the individual wanting to make improvements. IPT is an adaptive type of therapy.
Interpersonal psychotherapy (IPT) for depression is a time-limited treatment (12-16 weeks), with three phases:
1: Beginning (1-3 sessions) The first stage of treatment entails determining the target diagnosis (MDD) and the interpersonal environment in which it manifests.
2: Middle (6-12 sessions)
3: End (3 sessions)
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) is a medical therapy that has been used most often on patients with severe major depression who have failed to respond to other therapies. It includes the use of anesthetic and electrical brain stimulation during surgery.
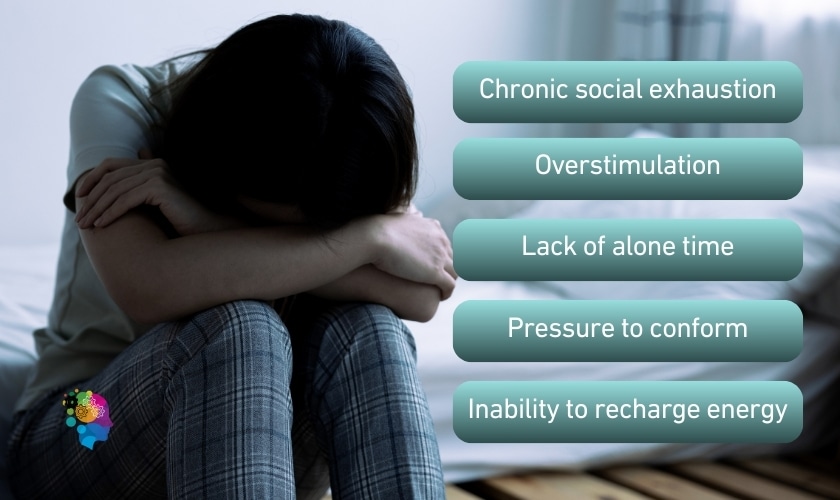
The importance of social support
Social support is an essential feature of social relationships. The goal of social support is always to be beneficial, distinguishing it from intentional negative encounters (such as critical criticism, nagging, or undermining).
Social support is commonly categorized into four types of behaviors.
- Emotional
- Instrumental
- Informational
- Appraisal
The importance of medication compliance
Patients with chronic conditions and complicated drug regimens are particularly susceptible to not taking their medications as prescribed.
U.S. Surgeon General C. Everett Koop, once reminded prescribers, patients, and pharmacists, “Drugs don’t work in patients who don’t take them.”
Medicines are undoubtedly one of the most important aspects of the treatment of MDD. For this reason, regular compliance with a medication regimen is critical for ensuring successful outcomes and minimizing serious adverse effects and even deaths.
Side effects of MDD
Major depression affects the way you eat and sleep. It affects the way you feel about yourself and those around you. It even affects your thoughts.
One of the most telling symptoms of MDD/Clinical depression is a change in sleep patterns. Though the most common side effect is insomnia (difficulty getting adequate sleep), people sometimes feel an increased need for sleep and experience excessive energy loss. Lack of sleep can cause some of the same symptoms as depression — extreme tiredness, loss of energy, and difficulty concentrating or making decisions.
Major depression can also cause weight gain or loss, despair and helplessness, and irritation. Treating depression helps the person to get control over all of these depression symptoms.
People with clinical depression are frequently involved in alcohol and drug addiction. They’re especially prevalent among teenagers and young and middle-aged males. It is very important to encourage these people to get help because they are more likely to attempt suicide.
Signs of drug and alcohol abuse include:
- Inability to maintain personal relationships
- Secretive alcohol use
- Self-pity
- Tremors
- Unexplained memory loss
- Unwillingness to talk about drugs or alcohol
Those who are depressed and abuse drugs or alcohol may require highly specialized therapy as soon as symptoms occur.
Suicidal thoughts
Warning signs of suicide with untreated depression
Warning signs of suicide include:
- Speaking, writing, or thinking about killing oneself or threatening to do so.
- Deep sadness, loss of interest, difficulty sleeping and eating, and worsening depression are some of the possible signs.
- Having a “death wish,” or tempting fate by taking chances that might result in death, such as driving through red lights and ignoring stop streets.
- One’s attention begins to wane when one no longer finds value in activities or things that were previously important.
- Making comments about being hopeless, helpless, or worthless.
- Putting things in order, finishing up loose ends, or updating a will are all other ways to say it.
- Saying things like “it would be better if I wasn’t here”
- A quick transition from being extremely sad to being very calm or seeming happy.
- Suddenly visiting or calling people one cares about.
- Talking about suicide.
- Increase in drinking alcohol or using drugs
- Writing a suicidal note
- Watching well-publicized murder and/or suicide reports in the media
- Online searches for methods to kill oneself are common.
Prevention techniques for MDD
Pets
Sometimes your pet can truly be your best friend, and it’s therapeutic. Playing with them lets you divert your thoughts from the issues that plague you. Taking care of them, help you to focus on something else outside yourself, which can be relaxing and can help to reduce your symptoms.
Eat smart
No specific foods treat depression, but a healthy diet can be part of an overall treatment plan. Build your meals and snacks around plenty of fruits, vegetables, and whole grains that also play a part in disease control.
Want to know how to eat healthier, then read our blog on The Lifestyle Guide to Being a Vegetarian.
Foods that boost your mood
Omega-3 fatty acids and vitamin B12 have been linked in studies to neurotransmitters that impact mood, as well as other brain processes. Low levels have been associated with sadness and depression.
Exercise to change how you feel
Exercise works almost as well as antidepressants for some people. And you don’t have to run a marathon. Just take a walk with a friend. As time goes on, move more until you exercise on most days of the week. You’ll feel better physically, sleep better at night, and boost your mood.
Exercise with others for support
Connections with other people can help you overcome the sluggish, lonely feelings of depression. Join an exercise group or work out with a friend. You’ll stay in touch and have support to keep yourself on track.
Get enough sunlight
Do you feel more depressed during darker, colder months? You may have seasonal affective disorder (SAD). It’s most common in the winter when there’s less sunlight. You can treat SAD with light therapy, antidepressants, Vitamin D supplements, and talk therapy.
Make time for mindful relaxation
Stress and anxiety can add to your depression symptoms and make it harder to recover. Learn to relax, and you can help restore a sense of calm and control. You might consider a yoga or meditation class. Or you could simply listen to soothing music while you take a long, warm bath.
Get involved in your community
When you spend time with people or causes you care about, you can regain a sense of purpose. And it doesn’t take much to get started. You can volunteer with a charity. Or join a discussion group at the library or at church. You’ll feel good about yourself when you meet new people and do new things.
Keep friends and family in your life
The people who love you want to support you. If you shut them out, they can’t. If you let them in, you’ll feel a lot better. Call a friend and go for a walk. Have a cup of coffee with your partner. You may find it helps to talk about your depression. It feels good to have someone listen.
Get the sleep you need
Depression makes it hard to get good rest. Some people sleep too much. Others can’t fall asleep easily. As you recover, relearn good nighttime habits. Start by going to bed and getting up at the same time each day. Use relaxation techniques to help you drift off. Quality shut-eye makes your mind and body feel better.
Struggling to sleep at night, try these melatonin supplements.
Avoid alcohol and drugs
They can slow your recovery from depression or stop it in its tracks. They can also make the condition worse and keep antidepressants from working well. If you have a problem with substance abuse, ask for help now. You’ll have a far better chance of getting past depression.
Conclusion
Exercise, a healthy diet, and other good habits may help you feel positive about your life. But they won’t replace medical treatment or talk therapy.
Depression is a serious illness, and it carries a risk of suicide. If you are thinking about harming yourself, get help right away. And never stop or change your treatment without discussing it with your doctor.
Major depression is an illness that involves the body, mood, and thoughts. It affects the way you eat and sleep. It affects the way you feel about yourself and those around you. It even affects your thoughts.
People who are depressed cannot simply “pull themselves together” and be cured. Without proper treatment, untreated clinical depression can last for weeks, months, or years.
FAQ
Can Depression Make You Sick?
Depression can make you feel sick and cause symptoms like exhaustion, headaches, nausea, and vomiting. It can also worsen preexisting medical conditions. Depression is a serious mental illness that requires treatment. If you think you may be depressed, please see a mental health professional.
Can Depression Cause Memory Loss?
Depression has been linked to memory problems, such as forgetfulness or confusion. While depression doesn’t cause memory loss, the two conditions may be related. Depression can make it difficult to focus and pay attention, which can lead to memory problems. Additionally, depression can lead to sleep problems, which can also contribute to memory difficulties.